A surprise party, a scary movie, chasing grandkids across the lawn – everyday situations can make your heart beat faster. But an abnormal rhythm that comes and goes could be a sign of atrial fibrillation (AF), a common heart issue that can affect your quality of life and even lead to serious issues like heart failure and stroke.
Understanding AF
Atrial fibrillation is an abnormal heart rhythm caused by electrical circuits in the heart, often affecting the upper chamber. Symptoms can include heart palpitations, shortness of breath, dizziness and swelling. Some people with AF can go on to develop heart failure because it stretches out the chambers of the heart and can cause leaking.
Not surprisingly, AF can have a real impact on quality of life. Yet many patients ignore symptoms or chalk them up to aging.
As an electrophysiologist, Dr. Monico Lo is an expert in the abnormal electrical signals that cause AF. You might think of her as an electrician for the heart. She helps prevent, manage and even resolve AF in patients of all ages, and sees firsthand how this issue can impact lives.
“You don’t want to ignore atrial fibrillation,” said Dr. Lo. “The most devastating thing I see is someone showing up with stroke and it’s their first diagnosis of AF.”
Diagnosing AF
In her AF practice, Dr. Lo sees patients from their teens to patients in their 90s and 100s. Some have a genetic predisposition for AF, some develop it over time and some experience sudden onset. AF is often associated with comorbidities, like sleep apnea, hypertension, diabetes and heart failure.
While AF is an issue that can affect people at any age, older patients are at higher risk. In fact, according to Dr. Lo, more than 20% of people over age 80 have AF.
“People might think that because they’re 60, they can’t do what they did at 30,” Dr. Lo said. “But people are living longer and longer, and we want to take care of those things.”
In younger patients, AF can be linked to thyroid issues, stimulants like caffeine and energy drinks, or binge drinking. Too much alcohol can stretch out the top chambers of the heart, which can trigger AF. Alcohol is also a diuretic, so too much can result in low potassium and low magnesium, causing an electrolyte imbalance that can trigger AF.
Regardless of the cause, detecting AF can be tricky. Since episodes come and go, doctors need to “catch it” happening, often with EKG or a heart monitor. But improved tracking methods are making AF detection easier.
Treating AF
The first step is to identify and address reversible causes or triggers. If AF is still an issue, the next step is management with a focus on reducing AF episodes and preventing stroke. An individualized care plan is key.
“We try to find a medication that is effective for that individual patient with the lowest side effect, based on their profile,” Dr. Lo said.
Patients can also have an ablation procedure. Ablation is a minimally invasive procedure that mainly targets veins from the lungs entering the left top chamber of the heart. It stops the abnormal electrical signals while still allowing flood flow. According to Dr. Lo, an ablation procedure can often resolve AF and get patients off of long-term medication.
“Sometimes it’s a combination of ablation and medication,” she said, “and sometimes we have to go in and touch up after ablation when the muscle fibers grow in and start firing those electrical signals again.”
Her recommendation? Take action on AF.
“The earlier we get hold of patients, the higher the success rate.”
Arkansas Heart Hospital offers atrial fibrillation and electrophysiology services through its Heart Rhythm Institute. You can also discover more heart health insights here to live a healthier and more proactive life.
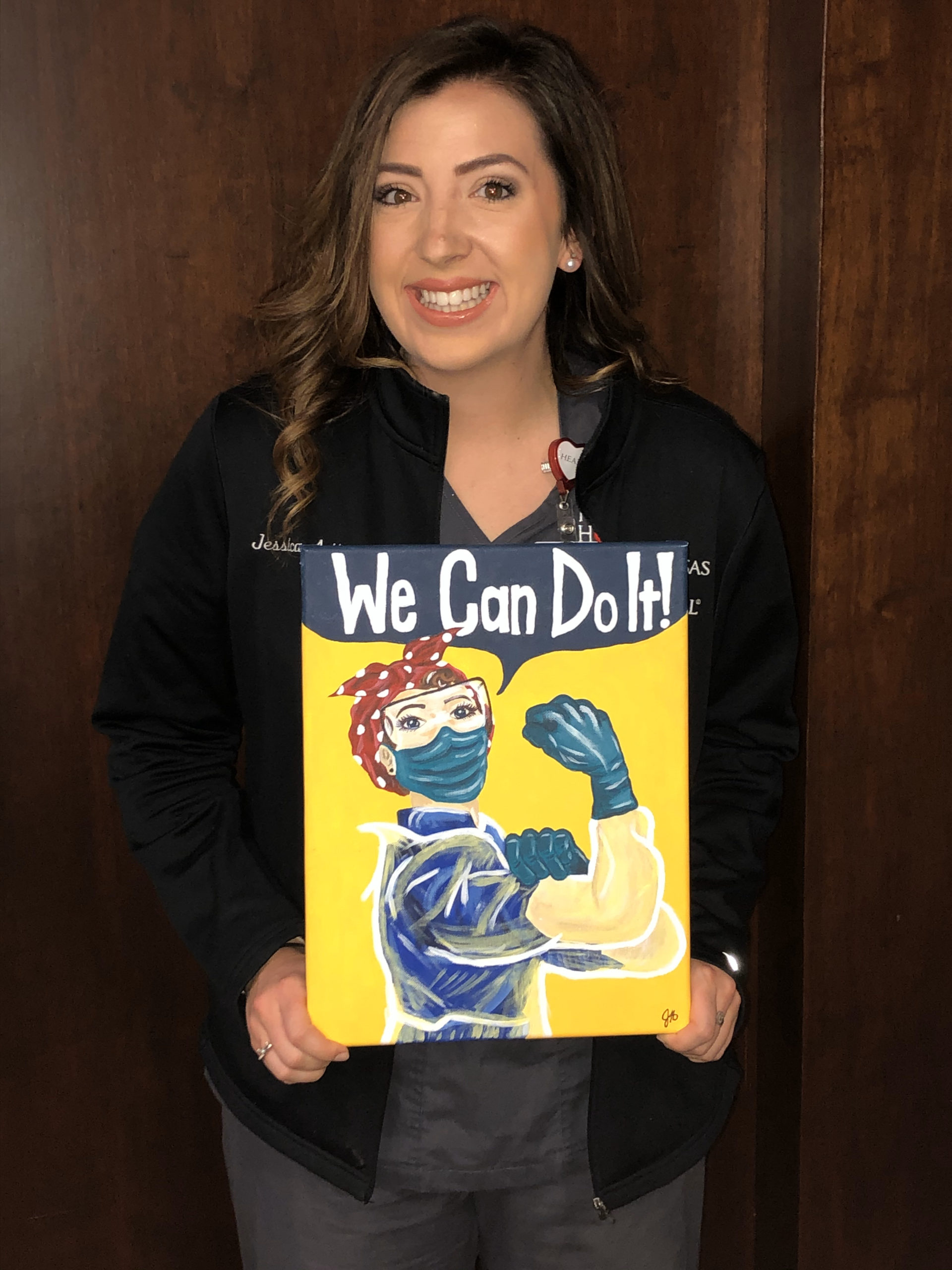 Jessica Adkins, a patient care partner on our COVID-19 team, quickly became an integral part of this “family within a family.” This team works alongside each other 12 hours a day, isolated from the rest of the hospital – a challenge on its own, but one that our team faces with grace and optimism. Every day brings something different, from revised CDC guidelines to revised hospital protocol, and the team relies heavily on each other to keep morale high.
Jessica Adkins, a patient care partner on our COVID-19 team, quickly became an integral part of this “family within a family.” This team works alongside each other 12 hours a day, isolated from the rest of the hospital – a challenge on its own, but one that our team faces with grace and optimism. Every day brings something different, from revised CDC guidelines to revised hospital protocol, and the team relies heavily on each other to keep morale high.